New tests help better stroke outcomes
Stroke patient rehabilitation can now be improved with a simple process that is helping therapists accurately predict how well their patients will regain the use of their hands and arms after a stroke.
University of Auckland researchers led by Associate Professor Cathy Stinear have created and tested a unique algorithm with therapists treating stroke patients at Auckland City Hospital.
The research is part of a wider study to better target stroke rehabilitation and improve patients' outcomes.
"The findings from the study showed that the algorithm could correctly predict how well stroke patients' hands and arms recovered in about 80 per cent of cases, something which is notoriously difficult to do otherwise," says Dr Stinear.
"What we've done is develop a simple algorithm that can make accurate predictions for individual patients, help therapists confidently tailor their therapy, and help patients leave hospital a week earlier with no negative effects on their recovery or satisfaction with care," she says.
The Health Research Council of New Zealand funded the study, and the findings were published online this month in the top international journal Stroke.
The algorithm, known as PREP for Predicting REcovery Potential, can be used in the initial days after a person has had a stroke, to predict if they will have an 'excellent', 'good', 'limited' or 'poor' recovery of their hand and arm.
"Your ability to live independently six months after a stroke depends on three main things: your age, the severity of the initial stroke, and how well your hand and arm recover movement," she says.
"We can't do anything about your age or how bad your stroke was, but we can do something about how we rehabilitate your hand and arm," says Dr Stinear.
Overseas research shows that therapists are not very good at predicting how well someone who has had a stroke will be using their hand and arm in three or six months' time, regardless of how much clinical experience they have.
Dr Stinear says there were particular difficulties predicting recovery in the middle group – people whose movement is not terrible, but not great either.
In this study, recovery predictions were provided for 110 stroke patients and withheld from 82 stroke patients in a comparison group.
Dr Stinear and her team found that therapists who used PREP were more confident that they knew what to expect for their patients' recovery.
This knowledge helped them to tailor their rehabilitation therapy to better meet each patient's individual needs. In turn, this helped their patients to leave hospital and get back to their homes a week earlier on average than patients who didn't receive the prediction information.
Using the PREP algorithm, the prognosis for close to two-thirds of stroke patients can be made with a simple two-minute clinical assessment of strength in a person's upper limb.
If patients score less than five out of ten on this test (about a third of patients), therapists then use a safe and non-invasive method called transcranial stimulation (TMS) to test how well messages are getting from the stroke side of the brain down to the muscles of the weak hand and arm.
"We've had patients who can't move their hand and arm at all, but when we use the TMS test and stimulate that movement area of their brain, we can see a response in those muscles.
"This tells us that even though things are looking pretty grim for that person at that point in time, they actually have great potential for recovery because the system still works," says Dr Stinear.
"This information helps us identify patients whose potential for recovery with intense therapeutic input might otherwise go unrecognised and unrealised. It's also really important for the patient and their family because it gives them hope and makes them more optimistic about recovery."
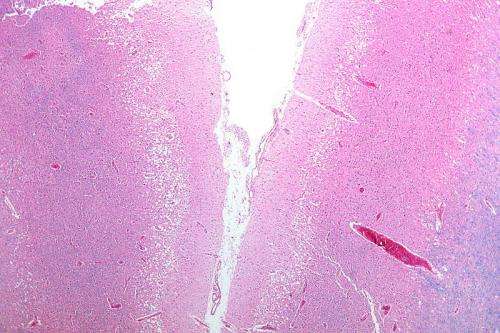
For patients who don't reach the required threshold in the TMS test, an MRI scan is used to see how much structural damage has been done to the key connections in their brain responsible for movement.
This can be used to predict if there are enough residual connections to get at least some movement back to help with basic things like dressing and bathing.
One possible concern was that people with a worse outlook might not be given as much rehabilitation, but Dr Stinear says this wasn't the case.
"The predictions didn't affect the amount of therapy that patients completed, only the goals and content of the therapy. Patients who received the prediction information recovered just as well those who didn't," she says.
Dr Stinear's HRC funding also supported neurological physiotherapist and doctoral student Marie-Claire Smith to run a parallel study for patients with walking difficulties after a stroke.
Ms Smith has created another algorithm that can predict when stroke patients will be able to walk independently again with more than 90 per cent accuracy and using just two simple clinical assessments.
More information: Cathy M. Stinear et al. Predicting Recovery Potential for Individual Stroke Patients Increases Rehabilitation Efficiency, Stroke (2017). DOI: 10.1161/STROKEAHA.116.015790


















